Credit: birthfaith.org
Someone I love gave birth last week for the first time. We talked on the phone about her experience a few days later. While she felt really good about how everything went, she was hurting. An episiotomy+tearing, back pain from her epidural, plus the normal pain associated with initiating breastfeeding were wearing on her. Having experienced some severe tearing with my first birth, I gave her my solidarity. Recovering from perineal trauma was some of the most excruciating physical pain I’ve ever experienced! I’d take labor pains over that any day.
During our phone conversation, she mentioned that one of the nurses at the hospital had asked her if she ate meat (she does eat a little, mostly chicken). Seems like a strange question, but apparently the nurses at that hospital had noticed a trend among the women they attended in labor: in their experience, women who were vegetarians were more likely to tear. A statement like that calls for some follow-up research, no? I jumped on it and starting digging around in the scientific literature to see what dietary substances are associated with increased skin elasticity. I never really found a clear-cut answer to the vegetarian question, but I did find lots of other cool information.
I’ve posted before about how to prevent tears from the outside in, but now I know a whole slew of ways we maybe able to protect our perineums from the inside out. These are some dietary additions you may want to make if you’re hoping to prevent tears (and improve your skin and health in general):
1. Healthy Fats
Earlier this year, Japanese researchers published their findings: “After controlling for covariates including age, smoking status, BMI and lifetime sun exposure, the results showed that higher intakes of total fat, saturated fat and monounsaturated fat were significantly associated with increased skin elasticity” (Source). The study also found that adding a high intake of green and yellow vegetables to that fat consumption improved skin health even further. That’s not to say we should eat just any fats. If you’re going to consume animal fats, your best bets are those coming from organic, grass-fed, free-range, or wild-caught animal sources. Plant sources of healthy fats, include olive oil, coconut oil, avocados, nuts, and seeds. Unfortunately, filler oils such as soybean oil are often added to many of the “olive oil” brands available. Find a reputable brand!
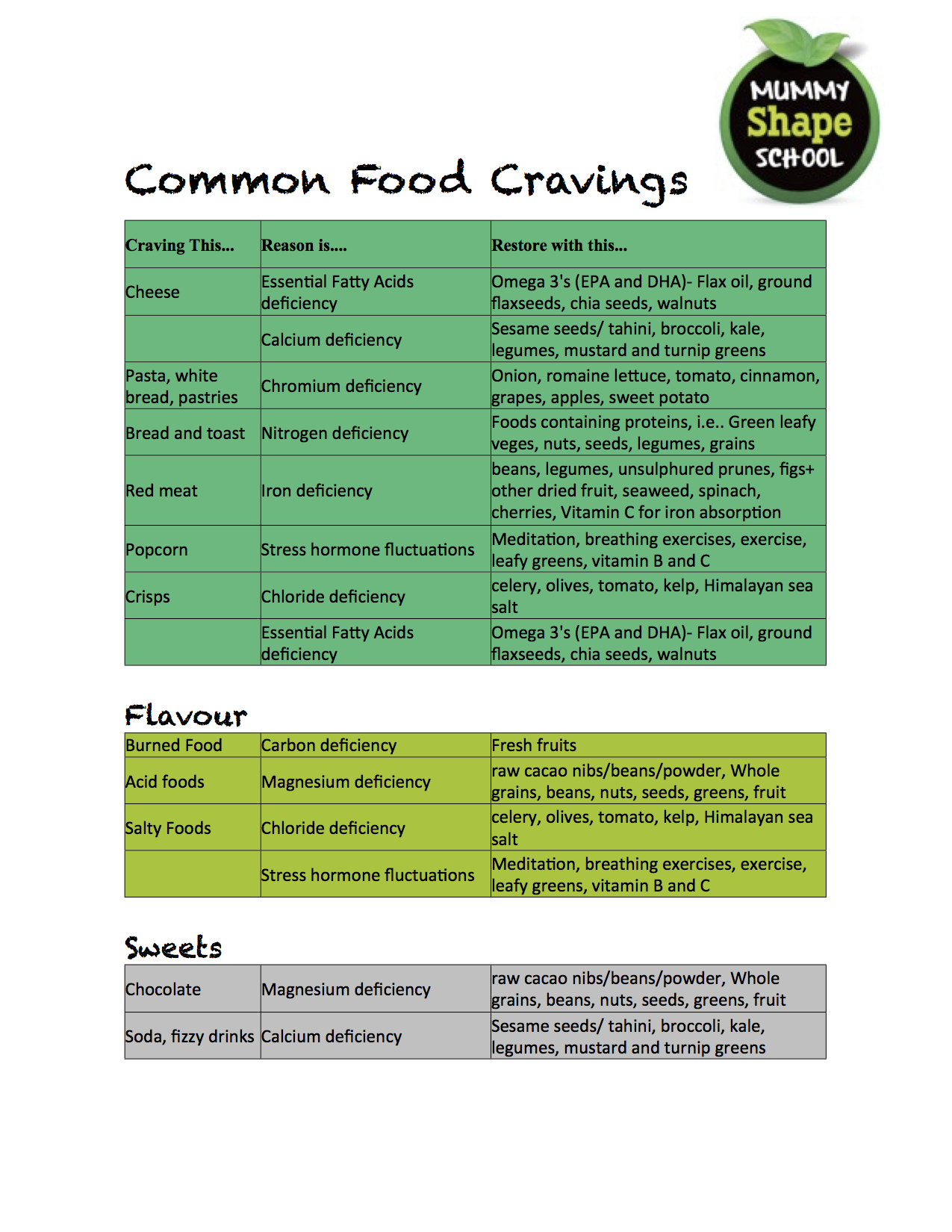
Then there are the fatty big guns: the omega-3s. Research indicates that supplementing with fish oil can significantly improve skin elasticity. Regularly consuming fatty fish like wild-caught salmon will also boost your omega-3 levels. Plant sources of omega-3 fatty acids include flaxseeds, chia seeds, pumpkin seeds, and walnuts. Personally, I try to eat from a wide variety of omega-3 sources to cover all my bases–DHA, EPA, and ALA.
Fats to limit/avoid: processed fats such as hydrogenated oils, trans fats, and any oils that go rancid easily… vegetable oils, corn oil, soybean oil, safflower oil, etc. Hydrogenated and rancid oils can lead to free radical damage which will reduce the health and elasticity of your skin (and contribute to a long list of other health problems).
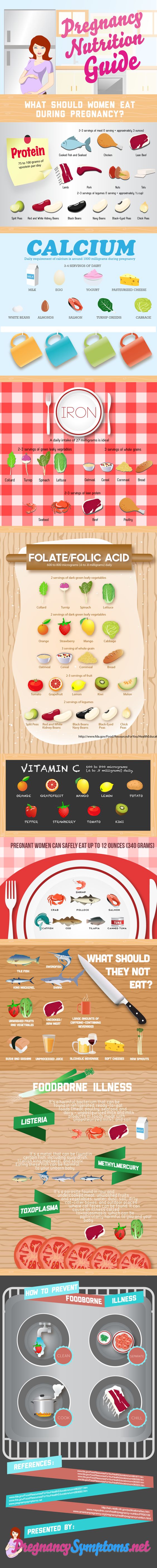
2. Vitamin C
“(Vitamin) C is for Collagen,” says Allison Tannis in her book Feed Your Skin, Starve Your Wrinkles. Collagen, she explains, “is a protein with a triple helix structure that provides a strong framework to support cells. Its tensile strength (the ability to resist force without tearing apart) is greater than that of steel, which explains why your skin is so strong” (p. 20). Or why your skin should be strong, that is. Reduced collagen levels lead to unhealthy, weak, aging skin. Vitamin C has been shown to stimulate collagen production (source). Logic would suggest, then, that increasing your intake of vitamin C would give your perineal skin added health and strength (a perineum of steel!) to resist trauma.
What are the best dietary sources of vitamin C? Papaya, red bell peppers, broccoli, brussel sprouts, and strawberries. Find morehere. Vitamin C will also boost collagen production (and overall health) when applied topically to the skin (source).
3. Cysteine
Now here’s where the vegetarians and vegans could be low. Cysteine is an amino acid as well as a powerful antioxidant. It promotes healthy skin elasticity and is necessary for skin repair. Most of the potent dietary sources of cysteine are animal products(meats, poultry, eggs, cottage cheese, yogurt, etc), but there are plant sources (red peppers, garlic, onions, broccoli, brussels sprouts, oats, granola, wheat germ) (source). Cysteine deficiencies are rare, but “strict amino acid-imbalanced vegetarian diets may lead to poor sulfur amino acid intake and [cysteine] deficiency signs” (source). Our bodies will actually produce cysteine on their own as long as enough methionine (another amino acid) is available. Vegans and vegetarians can pre-empt a cysteine deficiency by supplying their bodies with ample methionine. Good sources of methionine include eggs, fish, sesame seeds, brazil nuts, soy protein, parmesan cheese, meats, and cereal grains (see more here).
4. Evening Primrose Oil
A 2005 study found that adults taking capsules of evening primrose oil for twelve weeks had significantly improved skin elasticity, moisture, firmness, and fatigue resistance compared to adults taking a placebo (source). Evening primrose oil provides health-promoting forms of omega 6 essential fatty acids—linoleic acid (LA) and gamma-linolenic acid (GLA). While it has many medicinal uses, midwives have long encouraged evening primrose oil at the end of pregnancy as a means of ripening the cervix (through its prostaglandin content) for childbirth. Given that traditional usage, it may be wise to delay taking evening primrose oil until the 37th week of pregnancy and only in consultation with your maternity care provider. I’ve heard mixed reviews about whether it will help put you into labor, but research does indicate that it will improve the elasticity and health of your skin. I’ve also heard that it can be massaged into the perineum to prime the tissue to stretch well, and it is also supposed to be helpful when applied topically to prior perineal scars to loosen and soften them in preparation for a subsequent birth to prevent re-tearing.
5. Et Cetera
Other dietary additions that may benefit the strength and elasticity of your perineum…
- Silica—strengthens the skin and promotes elasticity and wound healing. Dietary sources: whole grains, dark leafy greens, leeks, green beans, garbanzo beans, strawberries, cucumber, mango, celery, asparagus and rhubarb.
- Selenium—promotes skin elasticity and prevents free radical cell damage. Dietary sources: brazil nuts are the most potent source (I hear you can even get too much selenium by eating more than a few per day), wheat germ, fish, garlic, eggs, brown rice, and whole-wheat bread.
- Vitamin E—promotes overall skin health and promotes wound healing. Dietary sources: sunflower seeds, almonds, olives, papaya, and dark leafy greens.
Other external preventative measures to reduce perineal trauma…
- Perineal massage during pushing stage (two fingers inside the vagina with a gentle sweeping motion to stretch the perineum). (Source) Massaging with lavender essence in the pushing stage has also been shown to prevent tears. (Source)
- Warm compresses (warm, wet cloths applied to the region during the pushing stage). (Source)
- Side-lying delivery position (lithotomy position increases tear risk). (Source)
- Optimal fetal positioning (abnormal cephalic presentations are associated with more severe perineal tearing). (Source) See these sites for tips on getting your baby into an ideal delivery position during the last weeks of pregnancy:
http://birthfaith.org/nutrition/protecting-your-perineum-from-the-inside-out